General Nuclear Imaging
Nuclear imaging is a branch of medical imaging that uses small amounts of radioactive material (tracer) to diagnose a variety of diseases, including many types of cancers, heart diseases, gastrointestinal, endocrine, neurological disorders and other abnormalities within the body. Because nuclear imaging procedures are able to pinpoint molecular activity within the body, they offer the potential to identify disease in its earliest stages as well as a patient’s immediate response to therapeutic interventions. Nuclear imaging procedures are invasive which means that the tracer is usually administered intravenously, rarely orally, taken with food or inhaled.
The route of administration depends on the type of nuclear imaging exam, and after the radiotracer is injected into the body, it eventually accumulates in the organ or area of the body being examined. Radioactive emissions from the tracer are detected by a gamma-camera.
-
What are some of the common uses of the procedure?
Physicians use radionuclide imaging procedures to visualize the structure and function of an organ, tissue, bone or system within the body. In adults, nuclear medicine is used to:
Heart
• visualize heart blood flow and function (such as a myocardial perfusion scan)
• detect coronary artery diseaseand the extent of coronary stenosis
• assess damage to the heart following a heart attack
• evaluate treatment options such as bypass heart surgery and angioplasty
• evaluate the results of revascularization procedures
• detect heart transplant rejection
• evaluate heart function before and after chemotherapy (MUGA)
Lungs
• scan lungs for respiratory and blood flow problems
• assess differential lung function for lung reduction or transplant surgery
• detect lung transplant rejection
Bones
• evaluate bones for fractures, infection and arthritis
• evaluate for metastatic bone disease
• evaluate painful prosthetic joints
• evaluate bone tumors
• identify sites for biopsy
Brain
• investigate abnormalities in the brain, such as seizures, memory loss and abnormalities in the blood flow
• detect the early onset of neurological disorders such as Alzheimer disease
• plan surgery and localize seizure foci
• evaluate for abnormalities in the brain involved in controlling movement in patients with suspected Parkinson’s disease
• evaluation of brain tumor recurrence, surgical or radiation planning or localization for biopsy
Other Systems
• identify inflammation or abnormal function of the gallbladder
• identify bleeding into the bowel
• assess post-operative complications of gallbladder surgery
• evaluate lymphedema
• evaluate fever of unknown origin
• locate the presence of infection
• measure thyroid function to detect an overactive or underactive thyroid
• help diagnose hyperthyroidism and blood cell disorders
• evaluate for hyperparathyroidism
• evaluate stomach emptying
• evaluate spinal fluid flow and potential spinal fluid leaks
Cancer
• stage cancer by determining the presence or spread of cancer in various parts of the body
• localize sentinel lymph nodes before surgery in patients with breast cancer or skin and soft tissue tumors
• plan treatment
• evaluate response to therapy
• detect the recurrence of cancer
• detect rare tumors of the pancreas and adrenal glands
Renal
• analyze native and transplant kidney function
• detect urinary tract obstruction
• evaluate for hypertension related to the kidney arteries
• evaluate kidneys for infection versus scar
• detect and follow-up urinary reflux
-
How should I prepare?
You may be asked to wear a gown during the exam or you may be allowed to wear your own clothing.
Women should always inform their physician or technologist if there is any possibility that they are pregnant or if they are breastfeeding.
You should inform your physician and the technologist performing your exam of any medications you are taking, including vitamins and herbal supplements. You should also inform them if you have any allergies and about recent illnesses or other medical conditions.
Jewelry and other metallic accessories should be left at home if possible, or removed prior to the exam because they may interfere with the procedure.
You will receive specific instructions based on the type of the scan you are undergoing. In some instances, certain medications or procedures may interfere with the examination ordered. Please refer to a specific Nuclear Imaging test overview for a detailed preparation guide.
-
What does the equipment look like?
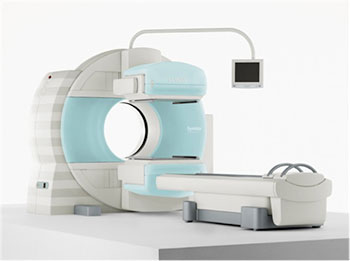 Special camera used in nuclear imaging include the gamma camera and single-photon emission-computed tomography (SPECT).
Special camera used in nuclear imaging include the gamma camera and single-photon emission-computed tomography (SPECT).The gamma camera, also called a scintillation camera, detects radioactive energy that is emitted from the patient’s body and converts it into an image. The gamma camera does not emit any radiation. The gamma camera is composed of radiation detectors, called gamma camera heads, which are encased in metal and plastic and most often shaped like a box, attached to a round circular donut shaped gantry. The patient lies on the examination table which slides in between the parallel gamma camera heads which are suspended over the examination table and located beneath the examination table. Sometimes, the gamma camera heads are oriented at a 90 degree angle and placed over the patient’s body.
 SPECT involves the rotation of the gamma camera heads around the patient’s body to produce more detailed, three-dimensional images.
SPECT involves the rotation of the gamma camera heads around the patient’s body to produce more detailed, three-dimensional images.A probe is a small hand-held device resembling a microphone that can detect and measure the amount of the radiotracer in a small area of your body. Probes are used for thyroid uptakes scans.
-
How does the procedure work?
 With ordinary x-ray examinations, an image is made by passing x-rays through the patient’s body. In contrast, nuclear imaging procedures use a radioactive material, called a radiopharmaceutical or radiotracer, which is injected into the bloodstream, swallowed or inhaled as a gas. This radioactive material accumulates in the organ or area of your body being examined, where it gives off a small amount of energy in the form of gamma rays. Special cameras detect this energy, and with the help of a computer, create pictures offering details on both the structure and function of organs and tissues in your body.
With ordinary x-ray examinations, an image is made by passing x-rays through the patient’s body. In contrast, nuclear imaging procedures use a radioactive material, called a radiopharmaceutical or radiotracer, which is injected into the bloodstream, swallowed or inhaled as a gas. This radioactive material accumulates in the organ or area of your body being examined, where it gives off a small amount of energy in the form of gamma rays. Special cameras detect this energy, and with the help of a computer, create pictures offering details on both the structure and function of organs and tissues in your body.Unlike other imaging techniques, nuclear imaging exams focus on depicting physiologic processes within the body, instead of showing anatomy and structure. Areas of greater intensity, called “hot spots,” indicate where large amounts of the radiotracer have accumulated and where there is a high level of chemical or metabolic activity. Less intense areas, or “cold spots,” indicate a smaller concentration of radiotracer and less chemical activity.
-
How is the procedure performed?
You will be positioned on an examination table. If necessary, a nurse or technologist will insert an intravenous (IV) catheter into a vein in your hand or arm.
Depending on the type of nuclear medicine exam you are undergoing, the dose of radiotracer is then injected intravenously, swallowed or inhaled as a gas.
It can take anywhere from several seconds to several days for the radiotracer to travel through your body and accumulate in the organ or area being studied. As a result, imaging may be done immediately, a few hours later, or even several days after you have received the radioactive material.
When it is time for the imaging to begin, the camera or scanner will take a series of images. The camera may rotate around you or it may stay in one position and you will be asked to change positions in between images. While the camera is taking pictures, you will need to remain still for brief periods of time. In some cases, the camera may move very close to your body. This is necessary to obtain the best quality images. If you are claustrophobic, you should inform the technologist before your exam begins.
If a probe is used, this small hand-held device will be passed over the area of the body being studied to measure levels of radioactivity. Other nuclear imaging tests measure radioactivity levels in blood, urine or breath.
The length of time for nuclear imaging procedures varies greatly, depending on the type of exam. Actual scanning time for nuclear imaging exams can take from 20 minutes to several hours and may be conducted over several days.
When the examination is completed, you may be asked to wait until the technologist checks the images in case additional images are needed. Occasionally, more images are obtained for clarification or better visualization of certain areas or structures. The need for additional images does not necessarily mean there was a problem with the exam or that something abnormal was found, and should not be a cause of concern for you.
If you had an intravenous line inserted for the procedure, it will usually be removed unless you are scheduled for an additional procedure that same day that requires an intravenous line.
-
What will I experience during and after the procedure?
Except for intravenous injections, most nuclear medicine procedures are painless and are rarely associated with significant discomfort or side effects.
When the radiotracer is given intravenously, you will feel a slight pin prick when the needle is inserted into your vein for the intravenous line. When the radioactive material is injected into your arm, you may feel a cold sensation moving up your arm, but there are generally no other side effects.
When swallowed, the radiotracer has little or no taste. When inhaled, you should feel no differently than when breathing room air or holding your breath.
It is important that you remain still while the images are being recorded. Though nuclear imaging itself causes no pain, there may be some discomfort from having to remain still or to stay in one particular position during imaging.
Unless your physician tells you otherwise, you may resume your normal activities after your nuclear medicine scan. If any special instructions are necessary, you will be informed by a technologist, nurse or physician before you leave the nuclear medicine department.
Through the natural process of radioactive decay, the small amount of radiotracer in your body will lose its radioactivity over time. It may also pass out of your body through your urine or stool during the first few hours or days following the test. You should also drink plenty of water to help flush the radioactive material out of your body as instructed by the nuclear medicine personnel.
You will be informed as to how often and when you will need to return to the nuclear medicine department for further procedures.
-
Who interprets the results and how do I get them?
A radiologist or other physician who has specialized training in nuclear medicine will interpret the images and forward a report to your referring physician.
-
What are the benefits vs. risks?
Benefits
• Nuclear medicine examinations provide unique information—including details on both function and anatomic structure of the body that is often unattainable using other imaging procedures.
• For many diseases, nuclear medicine scans yield the most useful information needed to make a diagnosis or to determine appropriate treatment, if any.
• Nuclear imaging offers the potential to identify disease in its earliest stage, often before symptoms occur or abnormalities can be detected with other diagnostic tests.
• Because the doses of radiotracer administered are small, diagnostic nuclear medicine procedures result in relatively low radiation exposure to the patient, acceptable for diagnostic exams. Thus, the radiation risk is very low compared with the potential benefits.
Risks
• Nuclear diagnostic procedures have been used for more than five decades, and there are no known long-term adverse effects from such low-dose exposure.
• Allergic reactions to radiopharmaceuticals may occur but are extremely rare and are usually mild. Nevertheless, you should inform the nuclear medicine personnel of any allergies you may have or other problems that may have occurred during a previous nuclear medicine exam.
• Injection of the radiotracer may cause slight pain and redness which should rapidly resolve.
• Women should always inform their physician or radiology technologist if there is any possibility that they are pregnant or if they are breastfeeding.
-
What are the limitations of General Nuclear Imaging?
Nuclear medicine procedures can be time consuming. It can take several hours to days for the radiotracer to accumulate in the body part of interest and imaging may take up to several hours to perform, though in some cases, newer equipment is available that can substantially shorten the procedure time.
The resolution of structures of the body with nuclear medicine may not be as high as with other imaging techniques, such as CT or MRI. However, nuclear medicine scans are more sensitive than other techniques for a variety of indications, and the functional information gained from nuclear medicine exams is often unobtainable by other imaging techniques.
Applicable Tests
Abdominal Scintigraphy
 Nuclear medicine imaging is a branch of medical imaging that uses small amounts of radioactive material to diagnose and determine the severity of a variety of diseases, including many types of cancers, heart disease, gastrointestinal, endocrine, neurological disorders and other abnormalities within the body. Because nuclear medicine procedures are able to pinpoint molecular activity within the body, they offer the potential to identify disease in its earliest stages as well as a patient’s immediate response to therapeutic interventions.
Nuclear medicine imaging is a branch of medical imaging that uses small amounts of radioactive material to diagnose and determine the severity of a variety of diseases, including many types of cancers, heart disease, gastrointestinal, endocrine, neurological disorders and other abnormalities within the body. Because nuclear medicine procedures are able to pinpoint molecular activity within the body, they offer the potential to identify disease in its earliest stages as well as a patient’s immediate response to therapeutic interventions.
Abdominal scintigraphy is used to visualize structure and function of the abdominal cavity organs. With this study, multiple organs can be assessed for pathological findings or malfunction.
These studies are:
- Liver/spleen imaging
- Hepatobiliary scintigraphy
- Gastrointestinal bleeding
- Meckel’s diverticulum scintigraphy
- Oesophageal studies
These procedures are used less often nowadays, having largely been replaced by ultrasound, CT and MRI. However, some techniques remain effective for specific clinical indications.
-
Why the test is done?
For abdominal scintigraphy, indications are specific to a particular screening.
Liver/spleen
This study is performed to determine the size and shape of the liver and spleen as well as for detecting functional abnormalities of the reticuloendothelial cells of these organs. Occasionally, the study is performed for:
· Suspected focal nodular hyperplasia of the liver.These lesions often have normal or increased uptake on sulphur colloid imaging.
· Assessments of reticuloendothelial system (RES) function in patients with suspected liver disease. The decision to perform a liver biopsy or to continue treatment with a hepatotoxic agent may be influenced by the severity of the liver disease that is seen on liver-spleen imaging as a complement to blood tests.
· Detecting functional splenic tissue.
· Adults with recurrent thrombocytopenia previously treated by splenoctomy.
· Characterization of an incidentally noted mass as functional splenic tissue.
· Evaluation of abdominal trauma with suspected splenic rupture.
· Viability assessment of splenic grafts.
Hepatobiliary scintigraphy
The study evaluates hepatocellular function and patency of the biliary system by tracing the production and flow of bile from the liver through the biliary into the small intestine. Sequential images of the liver, biliary tree and intestinal tract are obtained. Computer acquisitions and analysis as well as pharmaceutical interventions are frequently employed. Clinical indication include but are not limited to the following:
· Functional assessment of the hepatobiliary system.
· Evaluation of integrity of the hepatobiliary tree.
· Investigation of: suspected acute cholecystitis, chronic biliary tract disorders, common bile duct obstruction, bile extravasation, atresia of the biliary tree (differential diagnosis in neonatal jaundice), patency of bilio-enteric surgical anastomosis, enterogastric reflux.
Gastrointestinal bleeding
Gastrointestinal bleeding can be upper, originating above the ligament of Treitz, or lower, distal to the ligament of Treitz. Frequent causes of upper gastrointestinal bleeding include esophageal varices, gastric and duodenal ulcers, gastritis, esophagitis, Mallory-Weiss tears or neoplasms. Causes of lower gastrointestinal haemorrhage include angiodysplasia, diverticula, neoplasms and inflammation. The goals of gastrointestinal bleeding scintigraphy are to locate the bleeding site and to determine which patients require aggressive treatment as opposed to those who can be medically managed.
Meckel’s diverticulum scintigraphy
A Meckel diverticulum is a vestigial remnant of the omphalomesenteric duct located in the ileum, about 50-80 cm from the ileocecal valve. About half of Meckel diverticuli contain gastric mucosa. Bleeding may result from ileal mucosal ulceration from acid secretion. 99mTc pertechnetate avidly accumulates in gastric mucosa and is the study of choice for identifying ectopic gastric mucosa in Meckel diverticulum.
Oesophageal studies
By using radionuclide techniques, the function of the oesophagus and the gastro-oesophagus junction, and the presence and severity of gastro-oesophageal reflux can be studied. The main advantages of the procedure. Oesophageal motility disorders usually present with dysphagia or chest pain (often mimicking ischaemic cardiac disease). The following symptoms and conditions often occur in combination:
· Reflux oesophagitis
· Hiatus hernia
· Oropharyngeal dysfunction
· Primary and secondary achalasia
· Diffuse oesophageal spasm
· Oesophageal atresia and structure
· Connective tissue disorders
· Other systemic, neurological and myopathic disorders.
-
How do I prepare?
Liver/spleen imaging: No special preparation is required.
Hepatobiliary scan: To permit gall bladder visualization, the patient must have fasted for a minimum of two and preferably four hours prior to administration of the radiopharmaceutical. If the patient has fasted for longer than 24 hours or is on total parental nutrition, a false positive study for cholecystitis may occur. Please inform the technologist if this is case.
Gastrointestinal bleeding: Upon arrival to the clinic, the blood pressure and heart rate will be checked to confirm that the patient is haemodynamically stable. Intravenous catheter might be in place so that hypotension can be rapidly treated. No other preparation is needed.
Meckel’s diverticulum scintigraphy: Two days before the procedure you will be asked to start taking a medicine that would allow a better scanning procedure.
Oesophageal studies: Patients are usually studied in fasting state.
Adrenal Scintigraphy
Despite the important anatomic and structural details provided by CT and MRI, scintigraphy using a variety of radiopharmaceuticals that exploit the unique characteristics of adrenal function and metabolism, offers high sensitivity and specificity for characterization of incidentally discovered adrenal masses.
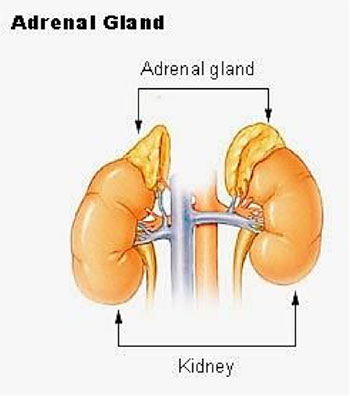 Types and uses of adrenal scintigraphy:
Types and uses of adrenal scintigraphy:
Iodocholesterol scintigraphy is used to depict adrenal adenomas and to distinguish adrenocortical carcinomas, metastases, cysts, hematomas, lipomas, myelolipomas and pseudoadrenal masses. The presence or absence of radiocholesterol uptake in an adrenal mass can be used to distinguish a benign from a space-occupying and potentially malignant adrenal lesion, whereas a normal pattern of imaging is seen in ‘epseudo’ adrenal masses. Planar scintigraphy has a limited spatial resolution of approximately 2 cm, such that lesions
NP-59, MIBG and FDG each target unique characteristics of adrenal gland function and can be used to assess the etiology of incidentally discovered adrenal masses. It is suggested that iodocholesterol imaging has positive and negative predictive values of 89% and 100%, respectively. Positive and negative predictive values for masses of adrenomedullary origin using MIBG were 83% and 100%, respectively, and [18F]-FDG separated benign from malignant adrenal lesions with 100% sensitivity and specificity.
If a functional imaging is used to evaluate an adrenal mass in patients with no history of cancer, iodocholesterol scintigraphy should be the logical first step because benign adenomas are the most common incidentally discovered adrenal masses; this approach should be followed by MIBG to identify nonhypersecreting pheochromocytoma, and [18F]-FDG if MIBG is non-localizing. Alternatively, in patients with malignancy or prior cancer history, [18F]-FDG should be the initial scintigraphic study followed by iodocholesterol and then MIBG.
-
What are common clinical indications for adrenal scintigraphy?
• Detection, localization, staging and follow-up of the following:
· Pheochromocytomas
· Neuroblastomas
· Ganglioneuroblastomas
· Ganglioneuromas
· Paragangliomas
· Carcinoid tumours
· Multiple endocrine neoplasia type 2 (MEN2) syndromes
• Assessment of uptake and residence time for treatment planning
• Evaluation of tumour response therapy
• Determination if high-dose 131-I-MIBG therapy may be beneficial
• Confirmation of suspected tumours arising from neuroendocrine tissue
• Evaluation of function of the adrenal medulla (hyperplasia)
-
Contraindications to the procedure
• Pregnant/breast-feeding • Interfering medications:
· Amphetamines
· Tricyclic antidepressants · Bretylium
· Calcium Channel blocking agents (e.g. Norvasc, Plendil, Cardene, Procardia etc.)
· Cocaine
· Guanethidine
· Haloperidol (Haldol)
· Labetalol (Trandate)
· Loxapine (Loxapac, Loxatine)
· Metaraminol (Aramine, Metaramin, Pressonex)
· Phenothiazines (Thorazine, Compazine)
· Reserpine (Serpalan)
· Sympathomimetics ( Ephedra, Ritalin)
· Thiothixene (Navane)
• Known hypersensitivity to iodine (low risk)
• Recent nuclear medicine study
-
How do I prepare?
• It is an absolute requirement that drugs which may interfere with the hypothalamic–pituitary–adrenal axis (e.g. glucocorticoids) or on the renin–angiotensin–aldosterone axis (e.g. spironolactone, most diuretics, sympathetic inhibitors, oestrogens) be discontinued to avoid distortion of the biodistribution and misinterpretation of the scintigraphic imaging. Please refer to the list of medications interfering medications listed above.
• You can eat and take medications as necessary (other than mentioned above).
• Please bring the list of your current medications for your appointment.
Bone Scan
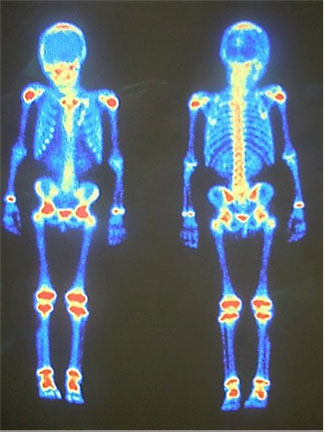 Skeletal scintigraphy (bone scan) is a special type of nuclear imaging procedure that uses small amounts of radioactive material to diagnose and determine the severity of a variety of bone diseases and conditions, including fractures, infections, and cancer.
Skeletal scintigraphy (bone scan) is a special type of nuclear imaging procedure that uses small amounts of radioactive material to diagnose and determine the severity of a variety of bone diseases and conditions, including fractures, infections, and cancer.
Because nuclear medicine procedures are able to image the functions of the body organs at the molecular level, they offer the potential to identify disease in its earliest stages as well as a patient’s immediate response to therapeutic interventions. In fact, a skeletal scintigram or bone scan can often find bone abnormalities much earlier than a regular x-ray exam.
-
Why is it done?
Physicians order skeletal scintigraphy to:
• find bone cancer or determine whether cancer from another area of the body, such as the breast, lung or prostate gland, has spread to the bones.
• diagnose the cause or location of unexplained bone pain, such as ongoing low back pain.
• help determine the location of an abnormal bone in complex bone structures, such as the foot or spine. Follow-up evaluation may then be done with a computed tomography (CT)or magnetic resonance imaging (MRI)
• diagnose broken bones, such as a stress fracture or a hip fracture, not clearly seen on x-rays.
• find bone damage caused by infection or other conditions, such as Paget disease.
-
How should I prepare?
You should inform your physician and the technologist performing your exam of any medications you are taking, including vitamins and herbal supplements and if you have allergies, have recently been ill or suffer from any other medical condition.
Women should always inform their physician or technologist if they are breastfeeding or if there is any possibility that they are pregnant.
Women who are breastfeeding will need to use formula for one to two days after the scan until the radioactive tracer is gone from their bodies. Be sure to dispose of any breast milk during this time.
You should inform the physician if you have taken a bismuth-containing medicine like Pepto-Bismol or if you have had an x-ray test using barium contrast material within the past four days. Barium and bismuth can interfere with bone scan results.
You will be asked to drink extra fluids after the radiotracer is injected, so limit your fluids for up to four hours before the test. You probably will have to wait several hours between injection of the tracer and the bone scan, so you may want to bring something to read or work on to pass the time.
You will be asked to wear a gown during the exam.
Jewelry and other metallic accessories should be left at home if possible, or removed prior to the exam because they may interfere with the procedure.
You will receive specific instructions based on the type of scan you are undergoing.
-
How is the procedure performed?
You will be positioned on an examination table. If necessary, a nurse or technologist will insert an intravenous (IV) catheter into a vein in your hand or arm.
It takes several hours for the tracer to circulate through your body and bind to your bones so that the pictures can be taken. During this time, you’ll be asked to drink four to six glasses of water to remove any unnecessary radiotracer that does not localize to the bones. You will also be asked to empty your bladder before the scan begins to prevent any tracer in the urine from blocking the view of your pelvic bones during the scan.
When it is time for the imaging to begin, the camera or scanner will take a series of images. The camera may rotate around you or it may stay in one position and you will be asked to change positions in between images. While the camera is taking pictures, you will need to remain still for brief periods of time. In some cases, the camera may move very close to your body. This is necessary to obtain the best quality images. If you are claustrophobic, you should inform the technologist before your exam begins.
The type of study you are having will determine the location of your injection and the number of scans performed. For some types of bone scans, pictures are taken during the tracer injection, immediately afterward, and then three to five hours after the injection. These types of exams are known as three-phase bone scans.
When the examination is completed, you may be asked to wait until the technologist checks the images in case additional images are needed. Occasionally, more images are obtained for clarification or better visualization of certain areas or structures. The need for additional images does not necessarily mean there was a problem with the exam or that something abnormal was found, and should not be a cause of concern for you.
Brain Scan and Cerebral Angiography

Brain Scan
The human brain is protected by several mechanisms. The skull provides bone coverage against outside impact and the blood-brain barrier (BBB) offers protection from toxic influence from the inside. The integrity of the BBB is broken as a consequence of a variety of brain lesions. Brain scan is a term referring to scintigraphic detection of the integrity of the BBB. Dynamic imaging of the head immediately after tracer injection, referred to as radionuclide cerebral angiography, depicts the cerebral vasculature.
Since the introduction of other imaging technologies with finer anatomical resolutions, such as CT, MRI or DSA (Digital subtraction angiography (DSA) is a type of fluoroscopy technique used in interventional radiology to clearly visualize blood vessels in brain), nuclear brain scanning is no longer the first choice to reveal an abnormality of the brain. However, in some clinical conditions, it remains a useful investigation.
-
Why is it done?
Diagnostic investigations are carried out for any of the following purposes:
• To detect the existence, location, extent and distribution of brain lesions (tumour, infarct, inflammation, haemorrhage or trauma) or intracranial lesions,
• To assess the integrity of the BBB in systemic disorders such as infection, intoxication or connective tissue diseases,
• To detect the patency and morphology of major intracranial vessels,
• To diagnose brain death.
Cerebral Perfusion Tomography (brain SPECT)
The human brain relies on continuous blood flow to supply all needed nutritional elements. Owing to the high extraction of oxygen from the blood, and the rapid adjustment of the blood flow to meet functional demands, the brain has a special mechanism to regulate its blood flow. This regulation is relatively independent of the systemic circulation and is determined by regional cerebral function and metabolism. This is sometimes referred to as the “trinity” of metabolism-function-flow of the brain. The perfusion, i.e. the distribution of blood supply at the tissue level of the brain, is a key aspect to revealing brain function.
Since the introduction of other imaging technologies with finer anatomical resolutions, such as CT, MRI or DSA (Digital subtraction angiography (DSA) is a type of fluoroscopy technique used in interventional radiology to clearly visualize blood vessels in brain), nuclear brain scanning is no longer the first choice to reveal an abnormality of the brain. However, in some clinical conditions, it remains a useful investigation.
-
Why is it done?
The purposes for which an investigation is needed include:
• Detection and evaluation of cerebrovascular disease:
· Differentiation of cerebral infarction
· Prediction of the outcome of patients with cerebrovascular accident (CVA)
· Work-up of patients with transient ischaemic attack (TIA)
• Evaluation of patients with suspected dementia
• Presurgical localization of epileptic foci
• Evaluation of symptomatic traumatic brain injury, especially in the absence of CT and/or MRI findings
• Diagnosis of encephalitis
• Monitoring and assessment of subarachnoid haemorrhage
• Verification of brain death
• Assistance in planning and monitoring treatment for intracranial or brain disorders.
Other indications include neuropsychiatric disorders such as depression, obsessive-compulsive disorder, chronic fatigue syndrome, neural degenerative diseases, for example Huntington’s chorea, and functional disorders, for example schizophrenia, where the findings of SPECT brain perfusion imaging have not been fully characterized. In HIV-positive encephalopathy, CO2 intoxication and connective tissue diseases, SPECT brain perfusion can detect organic changes in the brain and point to appropriate treatment and monitoring.
-
How do I prepare?
Patients will be instructed to stop taking caffeine, alcohol or other drugs known to affect cerebral blood flow (CBF) at least 1-3 days before the study. They will also be instructed to avoid smoking for at least the day of the test. Other medications should be discussed with a family physician.
You will be asked to sign a written consent for performing the procedure.
You will be asked to change into the clinic gown and void right before the procedure.
During the procedure you will be asked to keep your eyes closed or open, depending on the indication for the test and chosen protocol.
If the patients are unable to cooperate, (e.g. mental deficiency), sedation will be needed.
Gallium Scan
 A gallium scan is a nuclear imaging test. It uses small amount of radioactive material injected into the patient’s body to visualize the function and structure of internal body organs. Each type of tissue that may be scanned (including bones, organs, glands, and blood vessels) uses a different radioactive compound as a tracer. The radioactivity of a tracer decreases over a period of hours, days, or weeks. The tracer stays in the body until it is eliminated as waste, usually in the urine or stool (feces).
A gallium scan is a nuclear imaging test. It uses small amount of radioactive material injected into the patient’s body to visualize the function and structure of internal body organs. Each type of tissue that may be scanned (including bones, organs, glands, and blood vessels) uses a different radioactive compound as a tracer. The radioactivity of a tracer decreases over a period of hours, days, or weeks. The tracer stays in the body until it is eliminated as waste, usually in the urine or stool (feces).
During a gallium scan, the tracer (radioactive gallium citrate) is injected into a vein in the arm. It travels through the bloodstream and into the body’s tissues, primarily the bones, liver, intestine, and areas of tissue where inflammation or a build-up of white blood cells (WBCs) is present. It often takes the tracer a few days to build up in these areas, so in most cases a gallium scan is done at 2 days and again at 3 days after the tracer is injected. Areas where the tracer builds up in higher-than-normal amounts show up as bright or “hot” spots in the pictures. The problem areas may be caused by infection, certain inflammatory diseases, or a tumour.
-
Why is it done?
A gallium scan is done to:
• Detect the source of an infection that is causing a fever (called a fever of unknown origin).
• Detect an abscess or certain infections, especially in the bones.
• Monitor the response to antibiotic treatment.
• Diagnose inflammatory conditions such as pulmonary fibrosis or sarcoidosis (Sarcoidosis is a disease involving abnormal collections of inflammatory cells that can form as nodules in multiple organs).
• Detect certain types of cancer (such as lymphoma). A gallium scan also may be done to see if cancer has spread (metastasized) to other areas of the body, or to watch how well a cancer treatment is working.
-
How do I prepare?
Before the gallium scan, tell your doctor if:
• You are or might be pregnant.
• You are breast-feeding. If you will no longer be breast-feeding after the test, you will be asked to stop breast-feeding 2 weeks before the test so that the radioactive tracer will not build up in your breast tissue. If you will continue to breast-feed after the test, it is recommended that you not use your breast milk for 4 weeks after a gallium scan because the tracer can be passed to your baby. Some doctors may advise you to stop breast-feeding completely after this scan.
• Within the 4 days before the gallium scan, you have had an X-ray test using barium contrast material (such as a barium enema) or have taken a medicine (such as Pepto-Bismol) that contains bismuth. Barium and bismuth can interfere with test results.
• Gallium builds up in the large intestine (colon) before it is eliminated in the stool. You may need to take a laxative the night before the scan and have an enema 1 to 2 hours before the scan to prevent the gallium in your colon from interfering with pictures of the area being studied.
-
How is it done?
A gallium scan is usually done by a nuclear medicine technologist. The scan pictures are usually interpreted by a radiologist or nuclear medicine specialist.
The technologist cleans the site on your arm where the radioactive tracer will be injected. A small amount of the radioactive tracer is then injected. You will need to return for the diagnostic scans. Gallium scans are usually done 24 hours (1 day), 48 hours (2 days), and 72 hours (3 days) after the tracer is injected. It is absolutely necessary for you to come on a specific time for repeated scan.
When you come in for the scan, you will need to remove any jewellery that might interfere with the scan. You may need to take off all or most of your clothes, a gown will be given to use during the test.
You will lie on your back on a table, and a large scanning camera will be positioned closely above you. The camera does not produce any radiation, so you are not exposed to any additional radiation while the scan is being done.
Each scan may take about 60 to 90 minutes.
-
Risks
There is always a slight risk of damage to cells or tissue from being exposed to any radiation, including the low level of radiation released by the radioactive tracer used for this test.
Allergic reactions to the radioactive tracer are rare. Most of the tracer will be eliminated from your body (through your urine or stool) within 4 days. The amount of radiation is so small that it is not a risk for people to come in contact with you following the test.
-
Results
Normal: The collection and activity of gallium in the bones, liver, spleen, and large intestine (colon) is normal. No areas of unusual gallium accumulation are seen.
Abnormal: An abnormally high gallium accumulation (hot spot) is present in one or more areas of the body, possibly meaning inflammation, infection, or a tumour.
-
Limitations of the test
A gallium scan is used for specific types of cancers, mainly of the lymph nodes, bones, or bone marrow. A normal scan does not exclude the possibility of cancer, because some types of cancer do not show up on a gallium scan. A gallium scan also cannot determine whether a tumour is cancerous (malignant) or noncancerous (benign).
The results of a gallium scan should be interpreted along with the results of other tests, such as a physical exam, blood tests, and X-rays.
Gastric Emptying Scan
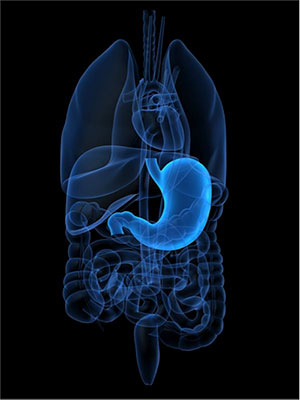 A gastric emptying scan, also known as a gastric emptying study or test, is a nuclear imaging test that uses a small amount of radioactive material (tracer) to determine how fast food leaves the stomach. The tracer, which travels through the gastric system, emits gamma energy which is detected by a special camera. The camera produces visual images with “cold” and “hot” spots of the areas with low or high tracer uptake.
A gastric emptying scan, also known as a gastric emptying study or test, is a nuclear imaging test that uses a small amount of radioactive material (tracer) to determine how fast food leaves the stomach. The tracer, which travels through the gastric system, emits gamma energy which is detected by a special camera. The camera produces visual images with “cold” and “hot” spots of the areas with low or high tracer uptake.
-
What is it done for?
Gastric emptying scans are often used to diagnose gastroparesis, a condition in which the stomach’s muscles don’t work properly. This results in a delay in sending food to the small intestine.
Doctors order the scans for adults who frequently vomit, feel bloated after eating, or complain of abdominal pain. Weight loss or changes in sugar levels are also symptoms of gastroparesis.
-
How the test is done?
 Gastric emptying scans take place at the special diagnostic clinics or hospitals. They are performed by professionals trained in nuclear medicine or radiology.
Gastric emptying scans take place at the special diagnostic clinics or hospitals. They are performed by professionals trained in nuclear medicine or radiology.Before the scan, the patient will eat a meal. This is usually scrambled eggs treated with a small amount of tasteless radioactive material. The radioactive substance allows the camera to follow the food through the digestive process.
The patient will lie on a table while the camera takes pictures. Every hour over the course of three to five hours, four to six scans lasting about a minute each will be taken.
It is important to remain still during the scan.
-
What are the risks of a gastric emptying scan?
A person will experience a small amount of radiation exposure from the material put in the food eaten before the scan. This is not considered dangerous, unless a woman is breast-feeding, pregnant, or planning to become pregnant. Anyone in these circumstances should tell her doctor before having a gastric emptying scan.
-
How do I prepare?
Other than the radioactive meal before the scan, patients should not eat or drink anything for four to six hours before the test.
It’s a good idea to bring books to read or a personal listening device to pass the time. Be sure to let the technician know if you are taking any medications or have any health complications, such as diabetes.
In-111 Leukocyte Scan
 In-111 leukocyte scintigraphy is a nuclear imaging test which displays the distribution of radiolabeled leukocytes in the body. Regional, whole-body, planar and/or SPECT scintigrams of specific anatomic regions are obtained for suspected infection/inflammation. In osteomyelitis (Osteomyelitis is an infection in a bone. Infections can reach a bone by traveling through the bloodstream or spreading from nearby tissue. Osteomyelitis can also begin in the bone itself if an injury exposes the bone to germs.), regional or whole-body bone scintigraphy may be used in conjunction with In-111 leukocyte scintigraphy to detect sites of abnormal bone remodeling. Bone marrow scintigraphy using Tc-99m sulfur colloid can be a useful adjunct to assess marrow distribution at suspected osteomyelitis sites, particularly when the site is adjacent to orthopaedic prostheses.
In-111 leukocyte scintigraphy is a nuclear imaging test which displays the distribution of radiolabeled leukocytes in the body. Regional, whole-body, planar and/or SPECT scintigrams of specific anatomic regions are obtained for suspected infection/inflammation. In osteomyelitis (Osteomyelitis is an infection in a bone. Infections can reach a bone by traveling through the bloodstream or spreading from nearby tissue. Osteomyelitis can also begin in the bone itself if an injury exposes the bone to germs.), regional or whole-body bone scintigraphy may be used in conjunction with In-111 leukocyte scintigraphy to detect sites of abnormal bone remodeling. Bone marrow scintigraphy using Tc-99m sulfur colloid can be a useful adjunct to assess marrow distribution at suspected osteomyelitis sites, particularly when the site is adjacent to orthopaedic prostheses.
Gallium scintigraphy is usually preferred in patients with:
(a) neutropenia
(b) fever of unknown origin; or
(c) non-suppurative or lymphocyte mediated infections. Technetium-99m HMPAO (Exametazime) labeled leukocyte scintigraphy is a frequently used option for acute infections, particularly in pediatric patients.
-
Why is it done?
• To detect sites of infection/inflammation in patients with granulocytosis and fever of unknown origin.
• To localize an unknown source of sepsis and to detect additional site(s) of infection in patients with persistent or recurrent fever and a known infection site.
• To survey for site(s) of abscess or infection in a febrile post-op patient without localizing signs or symptoms. Fluid collections, ileus, bowel gas and/or fluid, and healing wounds reduce the specificity of CT and ultrasound.
• To detect site(s) and extent of inflammatory bowel disease.
• To detect and follow-up osteomyelitis primarily when there is existing bone pathology such as infected joint prostheses, non-united fractures or sites of metallic hardware from prior bone surgery.
• To detect osteomyelitis in diabetic patients when degenerative or traumatic changes, neuropathic osteoarthropathy or prior osteomyelitis have caused increased bone remodeling.
• To detect osteomyelitis involving the skull in postoperative patients and for follow-up of therapy.
• To detect mycotic aneurysms, vascular graft and shunt infections.
-
How do I prepare?
Patients must be able to cooperate for whole body or regional scanning which may require 30–60 min for completion. No other special preparation for the test is needed.
-
How is it done?
In In-111 leukocyte scan, the white blood cells (mostly neutrophils) are removed from the patient, tagged with the radioisotope Indium-111, and then injected intravenously into the patient. The tagged leukocytes subsequently localize to areas of relatively new infection. The study is particularly helpful in differentiating conditions such as osteomyelitis from decubitus ulcers for assessment of route and duration of antibiotic therapy.
-
Limitations of the In-111 leukocyte scan
In imaging of infections, the gallium scan has a sensitivity advantage over the indium white blood cell scan in imaging osteomyelitis (bone infection) of the spine, lung infections and inflammation, and in detecting chronic infections. In part, this is because gallium binds to neutrophil membranes, even after neutrophil death, whereas localization of neutrophils labeled with indium requires them to be in relatively good functional order. However, indium leukocyte imaging is better at localizing acute (i.e., new) infections, where live neutrophils are still rapidly and actively localizing to the infection, for imaging for osteomyelitis that does not involve the spine, and for locating abdominal and pelvic infections.
Both the gallium scan and indium-111 white blood cell imaging may be used to image fever of unknown origin (elevated temperature without an explanation). However, the indium leukocyte scan will localize only to the approximately 25% of such cases which are caused by acute infections, while gallium is more broadly sensitive, localizing to other sources of fever, such as chronic infections and tumours. Gallium may be a better choice for spleen study because gallium does not normally accumulate in the spleen.
Lung Ventilation / Perfusion Scan
 A lung scan is a nuclear imaging test that is most commonly used to detect a blood clot that is preventing normal blood flow to part of a lung (to rule out pulmonary embolism).
A lung scan is a nuclear imaging test that is most commonly used to detect a blood clot that is preventing normal blood flow to part of a lung (to rule out pulmonary embolism).
Two types of lung scans are usually done together:
Ventilation scan: During a ventilation scan, a radioactive tracer gas or mist is inhaled into the lungs. Pictures from this scan can show areas of the lungs that are not receiving enough air or that retain too much air. Areas of the lung that retain too much air show up as bright or “hot” spots on the pictures. Areas that are not receiving enough air show up as dark or “cold” spots.
Perfusion scan: During a perfusion scan, a radioactive tracer substance is injected into a vein in the arm. It travels through the bloodstream and into the lungs. Pictures from this scan can show areas of the lungs that are not receiving enough blood. The tracer is absorbed evenly in areas of the lung where the blood flow is normal. These areas show up with the tracer distributed evenly. Areas that are not receiving enough blood show up as cold spots.
If the lungs are working normally, blood flow on a perfusion scan matches air flow on a ventilation scan. A mismatch between the ventilation and perfusion scans may indicate a pulmonary embolism.
Ventilation and perfusion scans can be done separately or together to diagnose certain lung diseases. If both scans are done, the test is called a V/Q scan. The ventilation scan usually is done first.
-
Why is it done?
A lung scan is done to:
• Find a blood clot that is preventing normal blood flow (perfusion) to part of a lung (pulmonary embolism).
• Check the flow of blood (perfusion) or air (ventilation) through the lungs.
• See which parts of the lungs are working and which are damaged. This is often done before lung surgery to remove parts of the lung.
-
How do I prepare?
Before your lung scan, tell your doctor if:
• You are or might be pregnant.
• You are breast-feeding. The radioactive tracer used in this test can get into your breast milk. Do not breast-feed your baby for 1 or 2 days after this test. During this time, you can give your baby breast milk you stored before the test, or you can give formula. Discard the breast milk you pump for the 1 or 2 days after the test.
• A chest X-ray is usually done the same day either before or after the lung scan.
You may be asked to sign a consent form.
Talk to your doctor about any concerns you have regarding the need for the test, its risks, how it will be done, or what the results will mean. To help you understand the importance of this test, fill out the medical test information form.
-
How is it done?
A lung scan is usually done by a nuclear medicine technologist. The scan pictures are usually interpreted by a radiologist or nuclear medicine specialist.
You will need to remove any jewellery that might interfere with the scan. You will be asked to change into the clinic patient gown.
During the scan, you will either lie on your back with the scanning camera positioned over or under your chest, or you will sit with the camera positioned next to your chest. The camera does not produce any radiation, so you are not exposed to any more radiation while the scan is being done.
Ventilation scan
For the ventilation scan, a mask will be placed over your mouth and nose. Or you may have a nose clip on your nose and a tube in your mouth that you use for breathing. You will inhale the tracer gas or mist through the mask or tube by taking a deep breath and then holding it. The camera will scan for radiation released by the tracer and produce pictures as the tracer moves through your lungs. You may be asked to breathe the gas in and out through your mouth for several minutes. You may then be asked to hold your breath for short periods (about 10 seconds) and to change positions so your lungs can be viewed from other angles. The camera may move to take pictures from different angles. You need to remain very still during the scans to avoid blurring the pictures.
Afterward, the radioactive gas or mist will clear from your lungs as you breathe.
The ventilation scan takes about 15 to 30 minutes.
Perfusion scan
For the perfusion scan, the technologist cleans the site on your arm where the radioactive tracer will be injected. A small amount of the radioactive tracer is then injected.
After the radioactive tracer is administered, the camera will scan for radiation released by the tracer and produce pictures as the tracer moves through your lungs. The camera may be repositioned around your chest to get different views. You need to remain very still during the scans to avoid blurring the pictures.
The perfusion scan takes about 5 to 10 minutes.
-
Results
Normal
The radioactive tracer is evenly distributed throughout the lungs during ventilation and perfusion.
Abnormal
The ventilation scan is abnormal but the perfusion scan is normal. This may mean abnormal airways in all or parts of the lung. Chronic obstructive pulmonary disease (COPD) or asthma may be present.
The perfusion scan is abnormal but the ventilation scan is normal. Depending on the difference between the two scans, a pulmonary embolism may be present.
Both the ventilation and perfusion scans are abnormal. This can be caused by certain types of lung disease, such as pneumonia, COPD, or a pulmonary embolism.
Myocardial Perfusion Imaging
 Myocardial perfusion imaging (MPI) is a nuclear imaging test that shows how well blood flows through (perfuses) your heart muscle. It can show areas of the heart muscle that aren’t getting enough blood flow. This test is often called a nuclear stress test. It can also show how well the heart muscle is functioning.
Myocardial perfusion imaging (MPI) is a nuclear imaging test that shows how well blood flows through (perfuses) your heart muscle. It can show areas of the heart muscle that aren’t getting enough blood flow. This test is often called a nuclear stress test. It can also show how well the heart muscle is functioning.
A radioactive tracer injected into the patient’s bloodstream lets doctors view heart function using a scanner called a SPECT (Single Photon Emission Computed Tomography) camera. Two sets of images are taken, one with the patient at rest and one with, when the heart is working (stressed).
There are two types of stress tests:
• Treadmill exercise test is the standard way to stress the heart.
• Drug-induced stress is used when a patient is unable to perform the exercise test due to a physical disability or other reason. The patient is given a drug which increases the caliber of the coronary arteries (vasodilatation) which increases blood flow to the heart as exercising would.
The patient’s doctor will determine which of the stress tests is appropriate. Both tests take two hours each to complete.
-
Why the test is done?
Physicians use cardiac nuclear medicine studies to help diagnose cardiac disease.
The indications may include:
• unexplained chest pain.
• chest pain brought on by exercise (called angina).
Cardiac nuclear medicine imaging is also performed:
• to visualize blood flow patterns to the heart walls.
• to evaluate the presence and extent of suspected or known coronary artery disease.
• to determine the extent of injury to the heart following a heart attack, or myocardial infarction.
• to evaluate the results of bypass surgery or other revascularization procedures designed to restore blood supply to the heart.
• in conjunction with an electrocardiogram (ECG), to evaluate heart-wall movement and overall heart function with a technique called cardiac gating.
Quick facts
• An MPI test examines blood flow through your heart during exercise on a treadmill (“physical stress”) and while you rest. If you can’t exercise well, you’ll get a medicine (“chemical/pharmacologic stress”) to increase the blood flow to your heart muscle as if you were exercising.
• The test uses radioactive material called tracers. Tracers mix with your blood and are taken up by your heart muscle as the blood flows through your heart arteries.
• A special “gamma” camera takes pictures of your heart to show how well your heart muscle is perfused (supplied with blood).
• The pictures will help your doctor see if your heart muscle is getting enough blood, or if blood flow is reduced to parts of the heart muscle because of narrowed arteries. MPI can also tell if there are areas of dead cells (scars) from a past heart attack. Some forms of MPI can also tell your doctor if portion of the heart muscle that isn’t working well after a heart attack has a chance of going back to normal and if a coronary stent is place or bypass surgery is done (“viability imaging”).
• The amount of radiation you get from an MPI test is small.
-
What are the risks of an MPI test?
MPI tests are generally safe for most people. MPI studies expose you to a low amount of gamma radiation. Experts disagree if X-rays at such low doses can cause cancer, but the possibility exists that no dose of X-rays, however low, is completely safe.
Don’t take the test if your risk for a heart attack is low, or if there is no other reason (chest discomfort) to think that you have heart trouble. If you’re pregnant or think you might be pregnant, or if you’re a nursing mother, tell your doctor before you have this test. It could harm your baby.
-
How should I prepare?
• You may be asked to wear a gown during the exam or you may be allowed to wear your own clothing.
• Women should always inform their physician or technologist if there is any possibility that they are pregnant or if they are breastfeeding.
• You should inform your physician and the technologist performing your exam of any medications you are taking, including vitamins and herbal supplements. You should also inform them if you have any allergies and about recent illnesses or other medical conditions.
• You should inform your physician if you have asthma or chronic lung disease or have problems with your knees, hips or keeping your balance, which may limit your ability to perform the exercise needed for this procedure.
• Jewellery and other metallic accessories should be left at home if possible, or removed prior to the exam because they may interfere with the procedure.
• You should avoid caffeine (caffeinated as well as decaffeinated coffee, hot and cold tea, caffeinated soft drinks and energy drinks, etc.) and smoking for up to 48 hours before your examination. Your physician or radiologist may give you more specific instructions.
• You should not eat or drink anything after midnight on the day of your procedure, but you may continue taking medications with small amounts of water unless your physician says otherwise. If you take beta-blocker medication (Inderal, metoprolol, etc.) you should specifically ask your physician about temporary discontinuation.
-
What happens during my MPI test?
Specially trained technicians usually perform the test under the supervision of a cardiologist.
The technician places small electrodes on your chest, arms and legs. The disks have wires that hook up to a machine to record your electrocardiogram (ECG). The ECG keeps track of your heartbeat during your test and is used to tell the camera when to take a picture.
You’ll wear a cuff around your arm to keep track of your blood pressure.
The technician will put an intravenous line (IV) in your arm.
You’ll exercise on either a treadmill.
If you cannot exercise, your IV line will be connected to a bag that has a medicine to increase the blood flow to your heart, similar to when you exercise, or make your heart go faster. This is called a chemical or pharmacologic stress test. These medicines may include adenosine, dipyridamole (Persantine) or dobutamine.
When you reach your peak activity level, you’ll stop and receive a small amount of radioactive material (tracer) through the IV line.
You’ll lie still on a table for 10- 30 minutes while the gamma camera takes pictures of your heart. Several scans are done during that time to provide pictures of thin slices of your entire heart from all angles. It’s very important to hold completely still with your arms above your head while the pictures are being taken.
During the resting part of the test, you’ll receive more radioactive tracer and another set of pictures will be taken. This set of images will be compared to the images taken after exercise or stress.
The test usually takes 2 hours.
-
What happens after my MPI test?
You can usually go back to your normal activities right away.
Drink plenty of water to flush the radioactive material from your body.
Make an appointment with your doctor to discuss the test results and next steps.
Nuclear Cardioangiography
 A MUGA scan (Multi Gated Acquisition Scan) is nuclear imaging test designated to evaluate the function of the right and left ventricles of the heart, thus allowing informed diagnostic intervention in heart failure. It is also called radionuclide angiography, radionuclide ventriculography, or gated blood pool imaging, as well as SYMA (SYnchronized Multigated Acquisition) scan. This modality uniquely provides a cine image of the beating heart, and allows the interpreter to determine the efficiency of the individual heart valves and chambers. MUGA/Cine scanning represents a robust adjunct to the now more common echocardiogram.
A MUGA scan (Multi Gated Acquisition Scan) is nuclear imaging test designated to evaluate the function of the right and left ventricles of the heart, thus allowing informed diagnostic intervention in heart failure. It is also called radionuclide angiography, radionuclide ventriculography, or gated blood pool imaging, as well as SYMA (SYnchronized Multigated Acquisition) scan. This modality uniquely provides a cine image of the beating heart, and allows the interpreter to determine the efficiency of the individual heart valves and chambers. MUGA/Cine scanning represents a robust adjunct to the now more common echocardiogram.
-
Why is it done?
MUGA is typically ordered for the following patients:
• With known or suspected coronary artery disease (CAD), to diagnose the disease and predict outcomes
• With lesionsin their heart valves
• With congestive heart failure
• Who have undergone percutaneous transluminal coronary angioplasty, coronary artery bypass graftsurgery, or medical therapy, to assess the efficacy of the treatment
• With low cardiac outputafter open-heart surgery
• Who are undergoing cardiotoxicdrug agents such as in chemotherapyg., with doxorubicin or immunotherapy (herceptin)
• Who have had a cardiac transplant
-
How the procedure is done?
The MUGA scan is performed by labeling the patient’s red blood pool with a radioactive tracer, technetium-99m-pertechnetate (Tc-99m), and measuring radioactivity over the anterior chest as the radioactive blood flows through the large vessels and the heart chambers.
The tracer is administered to the patient with an IV. Then he is placed under a gamma camera, which detects the low-level gamma radiation being given off by technetium-99m. As the gamma camera images are acquired, the patient’s heart beat is used to ‘gate’ the acquisition. The final result is a series of images of the heart (usually sixteen), one at each stage of the cardiac cycle.
Depending on the objectives of the test, the doctor may decide to perform either a resting or a stress MUGA. During the resting MUGA, the patient lies stationary, whereas during a stress MUGA, the patient is asked to exercise during the scan. The stress MUGA measures the heart performance during exercise and is usually performed to assess the impact of a suspected coronary artery disease. In some rare cases, a nitroglycerin MUGA may be performed, where nitroglycerin (a vasodilator) is administered prior to the scan.
The resulting images show that the volumetrically derived blood pools in the chambers of the heart and timed images may be interpreted to calculate the ejection fraction and injection fraction of the heart. This nuclear medicine scan yields an accurate, inexpensive and easily reproducible means of measuring and monitoring the ejection and injection fractions of the ventricles, which are one of the important clinical metrics in assessing global heart performance.
-
How long does the procedure take?
MUGA test usually takes about one hour.
-
How should I prepare for the test?
• There is no special preparation required for this test; there are no medication or food restrictions.
• Wear comfortable lose-fitting clothes, as you may be asked to wear a hospital gown during the test.
• Wear running shoes in case of Stress MUGA needs to be performed.
Parathyroid Scan

A parathyroid scan is sometimes called a parathyroid localization scan or parathyroid scintigraphy. This scan uses radioactive pharmaceuticals that are readily taken up by cells in the parathyroid glands to obtain an image of the glands and any abnormally active areas within them.
-
Why is it done?
The parathyroid glands, embedded in the thyroid gland in the neck, but separated from the thyroid in function, control calcium metabolism in the body. The parathyroid glands produce parathyroid hormone (PTH). PTH regulates the level of calcium in the blood.
Calcium is critical to cellular metabolism, as well as being the main component of bones. If too much PTH is secreted, the bones release calcium into the bloodstream. Over time, the bones become brittle and more likely to break. A person with levels of calcium in the blood that are too high feels tired, run down, irritable, and has difficulty sleeping. Additional signs of too much calcium in the blood are nausea and vomiting, frequent urination, kidney stones and bone pain. A parathyroid scan is administered when the parathyroid appears to be overactive and a tumour is suspected.
-
How is it done?
A parathyroid scan is a nuclear imaging procedure that uses two radiopharmaceuticals (drugs with a radioactive tracers) to obtain an image of highly active areas of the parathyroid glands. The test can be done in two ways.
1. Immediate scan
If the test is to be performed immediately, the patient lies down on an imaging table with his head and neck extended and immobilized. The patient is injected with the first radiopharmaceutical. After waiting 20 minutes, the patient is positioned under the camera for imaging. Each image takes five minutes. It is essential that the patient remains still during the imaging.
After the first imaging is done, the patient is injected with a second radiopharmaceutical, and imaging continues for another 25 minutes. Total time for the test is about one hour: injection 10 minutes, waiting period 20 minutes, and imaging 30 minutes.
Another way to do this test is as follows. After the first images are acquired, the patient returns two hours later for additional images. Time for this procedure totals about three hours: injection 10 minutes, waiting period two hours and 20 minutes, and imaging 30 minutes.
2. Delayed scan
In a delayed parathyroid scan, the patient is asked to swallow capsules containing the first radiopharmaceutical. The patient returns after a four hour waiting period, and the initial imaging is done. Then the patient is injected with the second radiopharmaceutical. Imaging continues for another 25 minutes. The total time is about four hours and 40 minutes: waiting period is four hours, injection 10 minutes, and imaging 30 minutes.
-
How do I prepare?
No special preparations are necessary for this test. It is not necessary to fast or maintain a special diet. The patient should wear comfortable clothing and no metal jewellery around the neck.
-
Risks
Parathyroid scans are not recommended for pregnant women because of the potential harm to the developing fetus. People who have had another recent nuclear medicine procedure or an intravenous contrast test may need to wait until the earlier radioactive markers have been eliminated from their system in order to obtain accurate results from the parathyroid scan.
-
Normal Results
Normal results will show no unusual activity in the parathyroid glands.
-
Abnormal Results
A concentration of radioactive materials in the parathyroid gland beyond background levels suggests excessive activity and the presence of a tumour. False positive results sometimes come from the presence of multinodular goiter, neoplasm, or cysts. False positive tests are tests that interpret the results as abnormal when this is not true.
Renal Scintigraphy
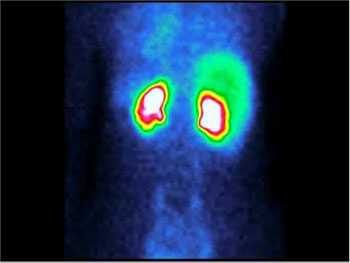 Renal scintigraphy, also known as “renal scanning” or “renal imaging,” refers to several examinations using radioisotopes that evaluate the function and anatomy of the kidneys. Renal scintigraphy is one of many imaging methods used to evaluate the kidneys. Ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI) can also be used. Your doctor will determine which of these examinations will provide the best information about your kidneys.
Renal scintigraphy, also known as “renal scanning” or “renal imaging,” refers to several examinations using radioisotopes that evaluate the function and anatomy of the kidneys. Renal scintigraphy is one of many imaging methods used to evaluate the kidneys. Ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI) can also be used. Your doctor will determine which of these examinations will provide the best information about your kidneys.
Different types of renal scans are used to examine different aspects of the kidneys and kidney functioning; however, all of these procedures involve the injection of a radiotracer or radioisotope into the patient. Because the radiotracer accumulates differently in different kinds of tissues, it can help physicians determine if something is wrong with the kidneys. Renal scintigraphy can also be used to evaluate a transplanted kidney.
-
What are some common uses of the procedure?
Four types of renal imaging help determine whether the kidneys are working normally or abnormally.
Cortical renal scintigraphy detects the amount of functioning kidney tissue through images taken with a gamma camera approximately three hours after the injection of a radiotracer.
Renal perfusion and function imaging examines blood flow to the kidneys and identifies potential narrowing of the renal arteries. Through a series of images taken over 20 to 30 minutes immediately after radiotracer injection, it also helps determine how well the kidneys are functioning.
Diuretic renal scintigraphy detects kidney blockages through images taken before and after the introduction of a diuretic to move urine through the kidneys.
ACE-inhibitor renal scintigraphy helps determine if the cause of a patient’s high blood pressure is coming from the kidneys by comparing kidney images before and after taking a blood pressure medication called an “ACE-inhibitor.”
These procedures can be valuable for identifying kidney failure and/or transplant-related complications, as well as discovering kidney-related injuries.
-
How should I prepare?
Preparation can vary widely based on the type of scan being conducted. You may be asked to drink extra fluid or possibly receive intravenous (IV) fluids. You may also be given a diuretic to increase urine production. In some cases, the bladder may need to remain empty during the scan, necessitating the insertion of a catheter. In other cases, you may be asked to go to the bathroom and empty your bladder prior to imaging. You also may be asked to discontinue use of some medications prior to your exam.
You may be asked to wear a gown during the exam or you may be allowed to wear your own clothing.
Women should always inform their physician or technologist if there is any possibility that they are pregnant or if they are breastfeeding.
You should inform your physician and the technologist performing your exam of any medications you are taking, including vitamins and herbal supplements. You should also inform them if you have any allergies and about recent illnesses or other medical conditions.
Also tell your physician if you are taking non-steroidal anti-inflammatories (NSAIDs).
Jewellery and other metallic accessories should be left at home if possible, or removed prior to the exam because they may interfere with the procedure.
You will receive specific instructions based on the type of scan you are undergoing.
-
What does the equipment look like?
 Special camera or imaging devices used in nuclear medicine include the gamma camera and single-photon emission-computed tomography (SPECT).
Special camera or imaging devices used in nuclear medicine include the gamma camera and single-photon emission-computed tomography (SPECT).The gamma camera, also called a scintillation camera, detects radioactive energy that is emitted from the patient’s body and converts it into an image. The gamma camera does not emit any radiation. The gamma camera is composed of radiation detectors, called gamma camera heads, which are encased in metal and plastic and most often shaped like a box, attached to a round circular donut shaped gantry. The patient lies on the examination table which slides in between the parallel gamma camera heads which are suspended over the examination table and located beneath the examination table. Sometimes, the gamma camera heads are oriented at a 90 degree angle and placed over the patient’s body.
SPECT involves the rotation of the gamma camera heads around the patient’s body to produce more detailed, three-dimensional images.
-
How is the procedure performed?
Prior to imaging, you will be injected with a small amount of radiotracer. Diuretic renal scintigraphy, ACE-inhibitor renal scintigraphy, renal perfusion and function imaging will typically begin imaging while the tracer is being administered. Cortical imaging requires a three hour delay after tracer administration for imaging to begin.
You will be positioned on an examination table. If necessary, a nurse or technologist will insert an intravenous (IV) catheter into a vein in your hand or arm.
When it is time for the imaging to begin, the gamma camera will take a series of images. The camera may rotate around you or it may stay in one position and you will be asked to change positions in between images. While the camera is taking pictures, you will need to remain still for brief periods of time.
Depending upon the type of procedure, renal imaging can last from 30 minutes to 2 hours.
-
What will I experience during and after the procedure?
You will feel a slight pin prick when the radiotracer is injected. After the injection, you could experience a brief metallic taste.
You will be asked to lie on your back and will need to remain as still as possible while the camera takes each picture.
It is important that you remain still while the images are being recorded. Though nuclear imaging itself causes no pain, there may be some discomfort from having to remain still or to stay in one particular position during imaging.
In some cases, the camera may move very close to your body. This is necessary to obtain the best quality images. If you are claustrophobic, you should inform the technologist before your exam begins.
When the examination is completed, you may be asked to wait until the technologist checks the images in case additional images are needed. Occasionally, more images are obtained for clarification or better visualization of certain areas or structures. The need for additional images does not necessarily mean there was a problem with the exam or that something abnormal was found, and should not be a cause of concern for you.
Unless your physician tells you otherwise, you may resume your normal activities after your nuclear medicine scan. If any special instructions are necessary, you will be informed by a technologist, nurse or physician before you leave the nuclear medicine department.
-
Who interprets the results and how do I get them?
A radiologist or other physician who has specialized training in nuclear medicine will interpret the images and forward a report to your referring physician.
-
What are the benefits vs. risks?
Benefits
The information provided by renal imaging is unique and often unattainable using other imaging procedures.
Renal imaging yields useful information needed to make a diagnosis or to determine appropriate treatment, if any.
Risks
Because the doses of radiotracer administered are small, diagnostic nuclear medicine procedures result in relatively low radiation exposure to the patient, acceptable for diagnostic exams. Thus, the radiation risk is very low compared with the potential benefits.
Allergic reactions to radiopharmaceuticals may occur but are extremely rare and are usually mild. Nevertheless, you should inform the nuclear medicine personnel of any allergies you may have or other problems that may have occurred during a previous nuclear medicine exam.
-
What are the limitations of renal imaging?
Renal images cannot differentiate between cysts and tumours.
Nuclear medicine procedures can be time-consuming. You will be informed as to how often and when you will need to return to the nuclear medicine department for further procedures.
The resolution of structures of the body with nuclear imaging may not be as clear as with other imaging techniques, such as CT or MRI. However, nuclear medicine scans are more sensitive than other techniques for a variety of indications, and the functional information gained from nuclear medicine exams is often unobtainable by any other imaging techniques.
Scrotal Scintigraphy
 Scrotal nuclear medicine scan is a study of the blood circulation in the scrotum using radioactive contrast agent to highlight obstruction.
Scrotal nuclear medicine scan is a study of the blood circulation in the scrotum using radioactive contrast agent to highlight obstruction.
-
Why is it done?
This test is used almost exclusively to differentiate infection in the testis (testicle) from twisting and infarction. Infection is called epididymitis because it mostly involves a collection of tubules on top of the testicle called the epididymis. Twisting of the testis shuts off its blood supply and is called testicular torsion. Both conditions cause a very painful, swollen testis on one side. Both occur most often in young men, although infection usually occurs at a slightly greater age. The infection increases the blood supply, and the torsion cuts off the blood supply. This is an ideal situation for a blood flow study.
The distinction is critically important, because testicular torsion must be untwisted immediately or the testis will die. On the other hand, epididymitis responds to antibiotics, and surgery might further injure it.
-
How is the procedure done?
A radioisotope, technetium-99m, combined in a chemical (pertechnate) is injected intravenously while the patient is under a special machine that detects radiation. This radiation detector, called a gamma camera, scans the scrotum at one minute intervals for about five minutes, then less often for another 10 or 15 minutes. It then creates a computer projection that reveals the isotope trace in the scrotum. Since both sides are scanned, even greater accuracy is obtained by comparison.
-
How do I prepare?
This procedure is usually done as an emergency to determine the need for immediate surgery. No special preparation is required.
-
Risks
The amount of radiation is so slight that even the sensitive testicular tissue is at minimum risk.
-
Normal Results
Blood flow appears unobstructed.
-
Abnormal Results
Three possible images appear.
They are:
• Increased blood flow indicating infection
• No blood flow indicating testicular torsion
• Blood flow illuminated in a “donut” shaped pattern that indicates torsion that has resolved itself within the last few days.
Thyroid Scan Uptake
 A thyroid scan is a type of nuclear medicine imaging. The radioactive iodine uptake test (RAIU) is also known as a thyroid uptake. It is a measurement of thyroid function, but does not involve imaging.
A thyroid scan is a type of nuclear medicine imaging. The radioactive iodine uptake test (RAIU) is also known as a thyroid uptake. It is a measurement of thyroid function, but does not involve imaging.
Nuclear imaging is a branch of medical imaging that uses small amounts of radioactive material to diagnose and determine the severity of or treat a variety of diseases, including many types of cancers, heart disease, gastrointestinal, endocrine, neurological disorders and other abnormalities within the body through the assessment of body organs functions. Because nuclear medicine procedures are able to pinpoint molecular activity within the body, they offer the potential to identify disease in its earliest stages as well as a patient’s immediate response to therapeutic interventions.
The thyroid scan and thyroid uptake provide information about the structure and function of the thyroid. The thyroid is a gland in the neck that controls metabolism, a chemical process that regulates the rate at which the body converts food to energy.
-
What are some common uses of the procedure?
The thyroid scan is used to determine the size, shape and position of the thyroid gland. The thyroid uptake is performed to evaluate the function of the gland. A whole-body thyroid scan is typically performed on people who have or had thyroid cancer.
A physician may request these imaging tests to:
• determine if the gland is working properly
• help diagnose problems with the thyroid gland, such as an overactive thyroid gland, a condition called hyperthyroidism, cancer or other growths processes
• assess the nature of a nodule discovered in the gland
• detect areas of abnormality, such as lumps (nodules) or inflammation
• determine whether thyroid cancer has spread beyond the thyroid gland
• evaluate changes in the gland following medication use, surgery, radiotherapy or chemotherapy
-
How should I prepare?
You may be asked to wear a gown during the exam or you may be allowed to wear your own clothing.
Women should always inform their physician or technologist if there is any possibility that they are pregnant or if they are breastfeeding.
You should inform your physician and the technologist performing your exam of any medications you are taking, including vitamins and herbal supplements. You should also inform them if you have any allergies and about recent illnesses or other medical conditions.
You should tell your physician if you:
• have had any tests, such as an x-ray or CT scan, surgeries or treatments using iodinated contrast material within the last two months.
• are taking medications or ingesting other substances that contain iodine, including kelp, seaweed, cough syrups, multivitamins or heart medications.
• have any allergies to iodine, medications and anesthetics.
• are breastfeeding.
In the days prior to your examination, blood tests may be performed to measure the level of thyroid hormones in your blood. You may be told not to eat for several hours before your exam because eating can affect the accuracy of the uptake measurement.
Jewelry and other metallic accessories should be left at home if possible, or removed prior to the exam because they may interfere with the procedure.
You will receive specific instructions based on the type of scan you are undergoing.
-
How is the procedure performed?
Thyroid Scan
You will be positioned on an examination table. If necessary, a nurse or technologist will insert an intravenous (IV) catheter into a vein in your hand or arm.
When radiotracer is taken by mouth, in either liquid or capsule form, it is typically swallowed up to 24 hours before the scan. The radiotracer given by intravenous injection is usually given up to 30 minutes prior to the test.
When it is time for the imaging to begin, you will lie down on a moveable examination table with your head tipped backward and neck extended. The gamma camera will then take a series of images, capturing images of the thyroid gland from three different angles. You will need to remain still for brief periods of time while the camera is taking pictures.
When the examination is completed, you may be asked to wait until the technologist checks the images in case additional images are needed. Occasionally, more images are obtained for clarification or better visualization of certain areas or structures. The need for additional images does not necessarily mean there was a problem with the exam or that something abnormal was found, and should not be a cause of concern for you.
If you had an intravenous line inserted for the procedure, it will usually be removed unless you are scheduled for an additional procedure that same day that requires an intravenous line.
Actual scanning time for a thyroid scan is 30 minutes or less.
Thyroid Uptake
You will be given radioactive iodine (I-123 or I-131) in liquid or capsule form to swallow. The thyroid uptake will begin several hours to 24 hours later. Often, two separate uptake measurements are obtained at different times. For example, you may have uptake measurements at four to six hours and 24 hours.
 When it is time for the imaging to begin, you will sit in a chair facing a stationary probe positioned over the thyroid gland in the neck.
When it is time for the imaging to begin, you will sit in a chair facing a stationary probe positioned over the thyroid gland in the neck.When the examination is completed, you may be asked to wait until the technologist checks the images in case additional images are needed. Occasionally, more images are obtained for clarification or better visualization of certain areas or structures. The need for additional images does not necessarily mean there was a problem with the exam or that something abnormal was found, and should not be a cause of concern for you.
Actual scanning time for each thyroid uptake is five minutes or less.
-
What are the limitations of the Thyroid Scan and Uptake?
The thyroid scan and thyroid uptake are not performed on patients who are pregnant because of the risk of exposing the fetus to radiation. These tests are also not recommended for breastfeeding women.
Nuclear imaging procedures can be time consuming. It can take several hours to days for the radiotracer to accumulate in the body part of interest and imaging may take up to several hours to perform.
The resolution of structures of the body with nuclear medicine may not be as high as with other imaging techniques, such as CT or MRI. However, nuclear medicine scans are more sensitive than other techniques for a variety of indications, and the functional information gained from nuclear medicine exams is often unobtainable by other imaging techniques.
Venography
 This test detects blood clots in the deep veins of the legs and blood flow patterns in the legs. Venography involves the injection of a small amount of a radioactive tracer into the foot veins of each leg. Pictures are taken to follow the blood flow up the legs.
This test detects blood clots in the deep veins of the legs and blood flow patterns in the legs. Venography involves the injection of a small amount of a radioactive tracer into the foot veins of each leg. Pictures are taken to follow the blood flow up the legs.
-
How do I prepare?
You should not wear elastic stockings for four hours prior to the test. Bring a list of all medications and supplements you take. This includes vitamins, herbal remedies, and holistic medications.
Any of these procedures is subject to change according to the nuclear medicine physician. The duration of the tests is a rough estimate. Please be aware that the time may be lengthened if a scan has to be repeated.
-
How long does the procedure take?
Venogram Using MAA: 45 minutes.
Venogram Using Labeled Red Blood Cells: one hour and 15 minutes.
-
How is the procedure performed?
Venogram Using MAA
A technologist will briefly explain the test to you and try to answer any questions you may have about the procedure. A technologist will ask you a few questions about your medical history and medications.
You will be asked to lie down on an imaging bed and a camera will be positioned above your legs. The technologist will inject a small amount of radioactive tracer into a vein in each foot. Pictures are taken during the injection and continue for a short time.
Venogram Using Labeled Red Blood Cells
A technologist will briefly explain the test to you and try to answer any questions you may have about the procedure. A technologist will ask you a few questions about your medical history and medications.
You will receive an injection of a blood labeling drug, which has no side effects, into a vein and then must wait 20 to 30 minutes. The technologist will ask you to lie down on the bed and the camera will be positioned above your legs.
The technologist will inject a small amount of radioactive tracer into a vein in each foot. Pictures are taken during the injection and continue for about 30 minutes.
